Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder
This study is a randomized clinical trial that investigated the use of psilocybin therapy as a treatment for Major Depressive Disorder (MDD). MDD is a significant global public health concern, affecting over 300 million individuals and causing substantial disability. The economic burden of MDD is estimated to be $210 billion in the United States. While existing pharmacotherapies for depression have limited efficacy and come with adverse effects, the study explores the potential of psilocybin therapy as a novel antidepressant intervention.
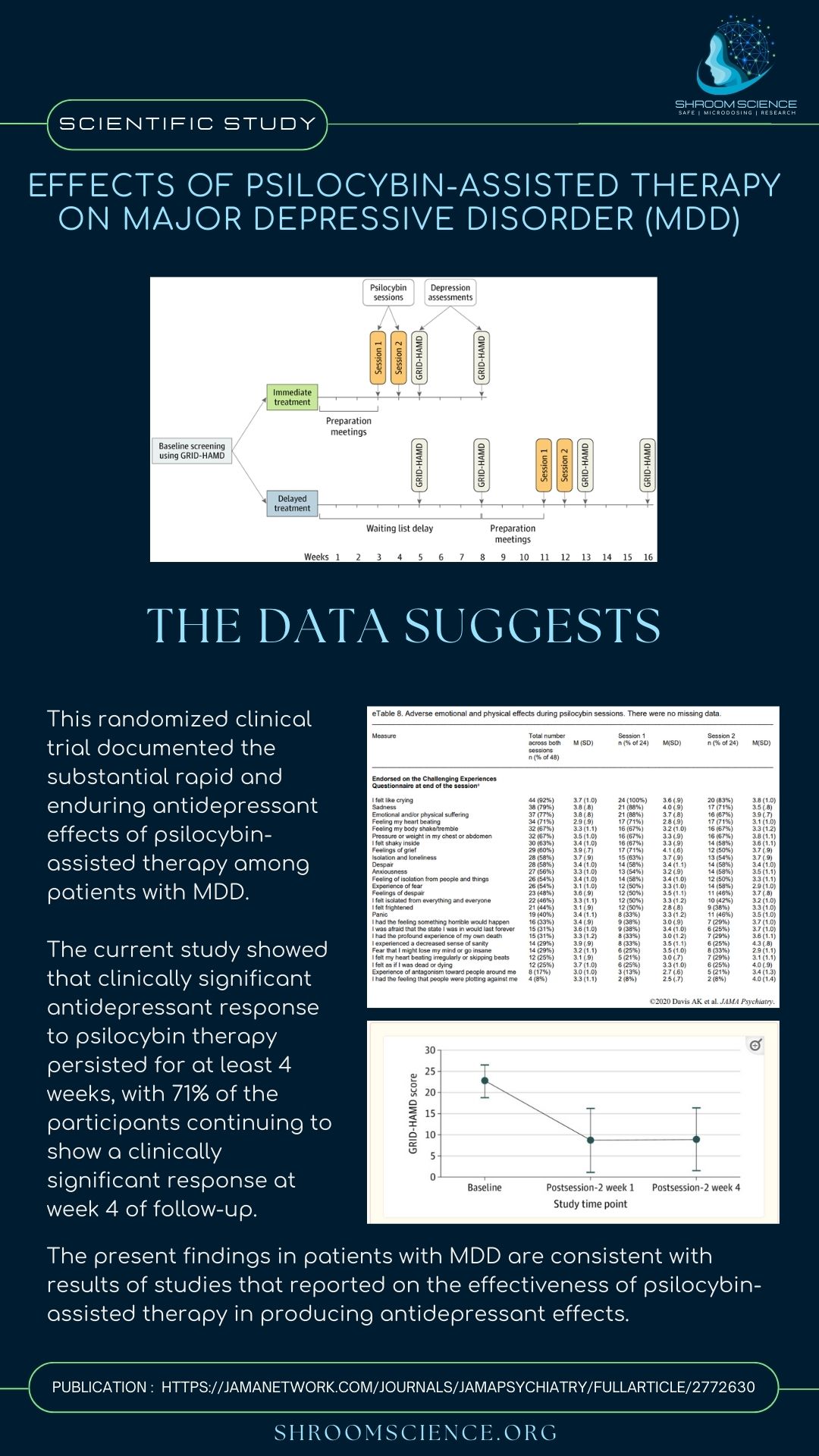
The research examines the efficacy of psilocybin therapy in patients with moderate to severe MDD. Participants aged 21 to 75 years, not currently on antidepressant medication, were included in the study. They underwent various screenings and assessments to ensure their suitability for the trial. The study employed a delayed treatment control group to differentiate the effects of psilocybin therapy from spontaneous symptom improvement.

Psilocybin Therapy for patients with Moderate to Severe MDD
The primary outcome measure was the GRID-Hamilton Depression Rating Scale (GRID-HAMD), a tool for assessing depression severity. The results showed rapid and sustained antidepressant effects of psilocybin therapy, with clinically significant responses persisting for at least four weeks. Notably, psilocybin was found to have low potential for addiction and a minimal adverse event profile, making it a promising alternative to ketamine.
The study also explored secondary depression and anxiety outcomes, revealing similar positive effects across multiple measures. Suicidal ideation was low and decreased in both groups. Psilocybin-occasioned mystical-type and insightful experiences were associated with decreased depression, suggesting a potential mechanism for its efficacy.
Psilocybin therapy produced significant improvements in depressive symptoms, surpassing the effectiveness of traditional psychotherapy and pharmacological treatments. The study’s findings support the idea that combined pharmacotherapy and psychotherapy may be more efficacious in treating MDD than either approach alone. Furthermore, psilocybin therapy was associated with mild-to-moderate adverse effects, such as headaches, during sessions, making it more acceptable to patients compared to common antidepressant medications with more problematic side effects.
However, the study has limitations, including a short-term follow-up, a relatively small and predominantly non-Hispanic White sample, and the absence of a placebo control group. Further research with larger, more diverse samples and longer-term follow-up is necessary to better understand the safety and efficacy of psilocybin therapy for MDD.

No Comments